Women in England will now be screened for cervical cancer every five years, instead of every three, health chiefs announced today.
The new protocol will be introduced from July, and applies to women aged 25 to 49 considered to be at low risk of the disease, which could amount to up to seven million people.
This comes following recommendations by the UK National Screening Committee and is already used for older women, aged 50 to 64 in England.
Modern cervical screening tests involve checking for an infection called human papillomavirus (HPV), which is the precursor to some 99 per cent of cervical cancers.
If a test is negative, women will now undergo no further testing for five years.
However those who test positive for HPV will continue to be invited for frequent check-ups to monitor any cell changes.
According to the NHS, studies have shown that if a woman tests negative for HPV, she is extremely unlikely to develop cervical cancer within the next decade.
Scientists at King’s College London said the new five-year approach is as effective as the traditional screening cycle, and identifies the same number of cancers despite less frequent testing.

The move to 5-year intervals brings England into line with Scotland and Wales, who have introduced this change following the UK National Screening Committee’s (UKNSC’s) recommendation
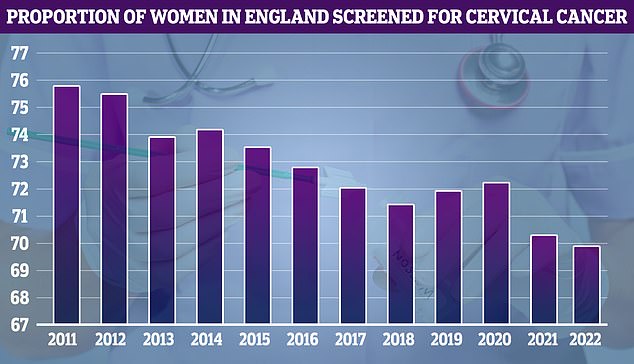
NHS cervical screening data, which goes back to 2011, shows uptake was at its highest that year (75.7 per cent) but has fallen over time
Campaigners have praised the move for making appointments, which can sometimes be uncomfortable, ‘easier to manage’.
‘Research last year showed many women can find it an uncomfortable experience, and sometimes difficult to schedule in around their busy lives,’ said Louise Ansari, Chief Executive of Healthwatch England.
‘Reducing the number of times they need to attend, alongside sensitive and empathetic approaches by health professionals, will make these important appointments easier to manage.’
During a cervical screening exam, a healthcare professional takes a swab of cells from inside the cervix to look for HPV.
If the virus, which is transmitted via sex, is detected, further lab tests are performed to check if the cells appear abnormal— and potentially cancerous—under the microscope.
If abnormal cells are found, women will be called back for a procedure called a colposcopy, whereby the cervix is examined further.
Those who have a positive HPV test but no abnormal cells will be monitored every year.
Most of the time HPV is harmless. But a handful of the 150 strains can, in some cases, invade the genital tract where it causes cells to mutate and turn cancerous.

Jade Goody, the former Big Brother contestant, tragically died in 2009 aged 27 from cervical cancer
Girls have been vaccinated against HPV at the age of 13 since 2008, and boys of the same age since 2019.
There are about 3,300 new cervical cancer cases—and 850 deaths—in the UK every year.
Perhaps the most high profile patient to fall victim to the disease is reality TV star Jade Goody, who died in 2009, aged 27, shortly after being diagnosed.
The star’s tragic death led to a temporary increase in women attending smear tests, although take-up of the test has declined in recent years.