US scientists have provided further evidence that blood tests can work to accurately diagnose dementia, by examining two proteins in blood plasma
A new blood test for Alzheimer’s disease can accurately detect people with early symptoms, according to research which experts hope to build on and bring us closer to a cure.
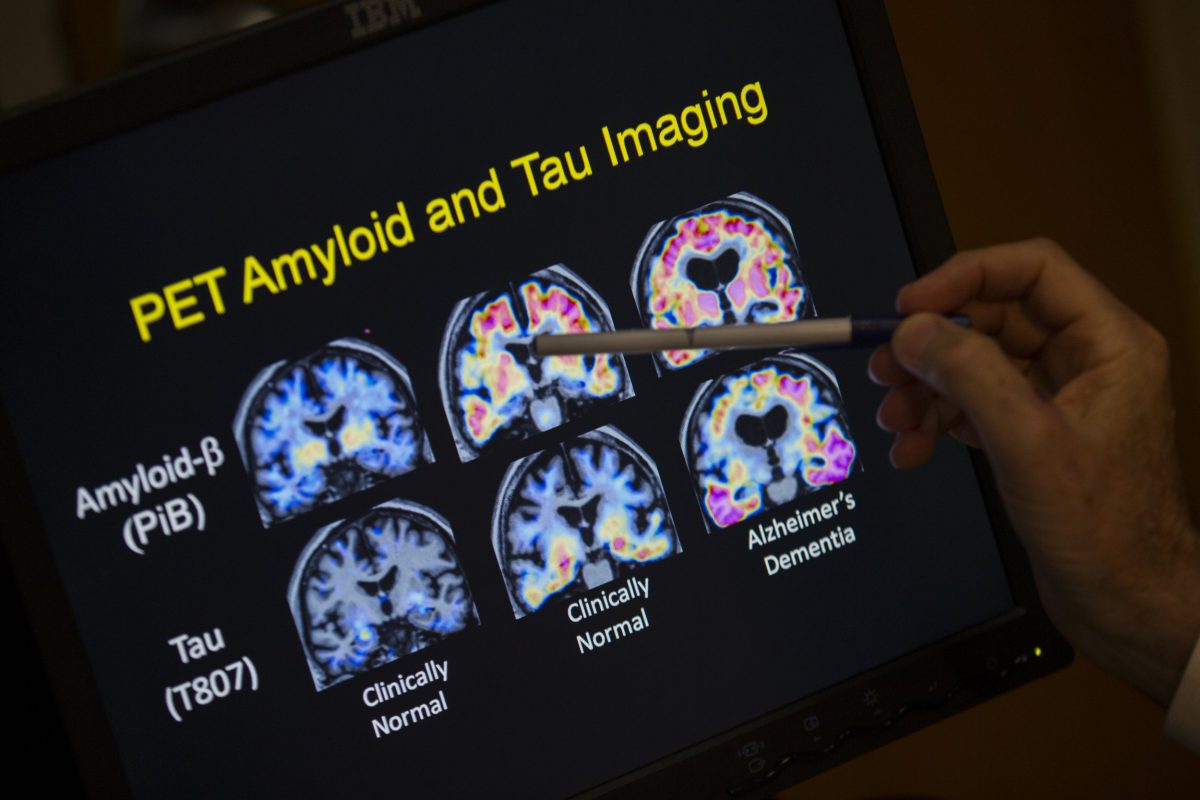
Scientists from the Mayo Clinic in the US have provided further evidence that blood tests can work to accurately diagnose dementia, by examining two proteins in blood plasma. These proteins – amyloid beta 42/40 and p-tau217 – are associated with amyloid plaque build-up, which is a hallmark of Alzheimer’s disease.
In the study of more than 500 people in an outpatient memory clinic, researchers found the blood test was both highly accurate (at 95 per cent) in detecting people with memory problems and in ruling out people without dementia (82 per cent). The blood test has already been approved by the Food and Drug Administration regulator in the US.
While not approved in the UK, the development will allow experts on the UK’s Blood Biomarker Challenge, a trial which hopes to bring dementia blood tests to the NHS within five years, to build on the research in the pursuit of finding adequate tests.
Dr Gregg Day, who led the study in the Alzheimer’s and Dementia journal, said the test was as good as more invasive tests currently in use, such as a lumbar puncture.
“Our study found that blood testing affirmed the diagnosis of Alzheimer’s disease with 95 per cent sensitivity and 82 per cent specificity,” he said.
“When performed in the outpatient clinical setting, this is similar to the accuracy of cerebrospinal fluid biomarkers of the disease and is much more convenient and cost-effective.”
Dr Richard Oakley, associate director for research and innovation at the Alzheimer’s Society in the UK, said the results “suggest this test is very accurate” and could be used alongside other tests and observations from a trained health professional.
Dr Oakley added: “Currently diagnosis options in the UK are often slow, expensive and can be invasive, meaning thousands miss out on the benefits one can bring. It’s great to see blood tests like this approved for clinical use in the US – we hope to see the same in the NHS, which is why we’re part of the Blood Biomarker Challenge.”
Overall, researchers found that p-tau217 levels were higher in patients with Alzheimer’s disease versus those without the disease. Dr Day said the next steps in the research were to evaluate blood-based testing in more diverse patient populations and people with early Alzheimer’s who show no cognitive symptoms.
The dementia drugs pipeline
An annual report published this week found there are 138 substances being tested globally, which target different aspects of dementia. The number of drugs entering early-stage trials has risen from 27 last year to 48 this year.
However, families should not expect new treatments imminently, as drugs can take 10 to 15 years to progress from the earliest stage of trials to reach the clinic. And most of the drugs are in early-stage trials, which often find the medicine fails to work, said Professor Rob Howard, a professor of old age psychiatry at University College London.
The two existing medicines for Alzheimer’s that help alleviate symptoms do not tackle the biological cause, but seem to help brain cells work more effectively. Several other drugs are being tested for this effect, making up 14 per cent of the research pipeline. There are other drugs in development that are aimed to ease the behavioural symptoms of Alzheimer’s, such as agitation and aggression.
A nationwide clinical trial is now underway in the UK is aiming to revolutionise how dementia is diagnosed. Research teams will assess how blood tests could be used to detect dementia at various stages.
“While focused on Alzheimer’s disease, the test was evaluated in people with other types of dementias too, showing that it may help to differentiate causes of cognitive decline – though more research in diverse groups of individuals and in community-based settings is still needed,” Dr Oakley said.
“Blood tests will be critical to accelerate diagnosis and give more people access to the care, support and treatments they desperately need faster than ever before. We must see long-term investment in the tools and workforce needed to ensure everyone living with dementia can get an early an accurate diagnosis, which is even more important with disease-modifying treatments on the horizon.”
Dr Julia Dudley, head of research at Alzheimer’s Research UK, said the latest study adds to the growing evidence that blood tests can detect the diseases that cause dementia in people with early memory and thinking problems.
“An important point to consider is that people taking part in research don’t always reflect the full diversity of those affected by dementia, who might have additional conditions or other characteristics. That is why work is needed to understand whether these blood tests work in a real-world setting,” she said.
“In the UK, studies like the Blood Biomarker Challenge are helping to build this evidence. The study is testing blood tests, including p-tau217, in thousands of people from sites across the UK. This work will be a crucial part of making diagnosis easier and faster, which will bring us closer to a cure.”